
In healthcare, data is crucial for patient care, research, and system management. Accurate and comprehensive clinical data enables informed decision-making, improves patient outcomes, and enhances operational efficiency. While the importance of data is undeniable, its value is highly dependent on the standards governing its collection, storage, and usage within healthcare organisations. Data standards in healthcare ensure that data is consistent, accurate, and interoperable across different systems and institutions.
This is where technologies play a vital role; healthcare software development equips professionals with the tools needed to manage data effectively and ensure compliance with standards.
Navigating the landscape of health data standards
In April 2024, the European Parliament approved the European Health Data Space (EHDS) framework. It is the initiative by the European Union aimed at creating a common framework for healthcare data exchange across its member states.
- The EHDS focuses on several key goals:
-
- Interoperability and standartisation. Ensuring medical data can be seamlessly shared and understood across different systems, healthcare providers and countries.
- Enhanced data quality. Improving health data collection to support effective secondary use in research, policymaking, and innovation.
- Data safety and anonymity. Implementing high-security requirements to safeguard the data.
The healthcare industry uses various standards to work with critical data. However, the large number of these standards makes the process more complicated than it should be. As part of the European Health Data Space (EHDS), all healthcare organisations must ensure their data is interoperable. Unfortunately, the current framework does not specify which standards should be adopted. Interoperability, in this context, refers to the ability of different systems to exchange information securely.
Researchers opinion: healthcare data types and corresponding standards
Different data standards satisfy different needs, and no single standard can meet all healthcare system requirements. The scientific paper "Converge or Collide? Making Sense of a Plethora of Open Data Standards in Health Care" identifies three types of healthcare data: clinical care and administration, data exchange, and longitudinal analysis. Each of the types has specific standards to address:
- Clinical care and administration: Care documentation should capture a wide range of hospital data, including unexpected patient-related events. The OpenEHR standard can cover this.
- Data exchange: Healthcare data should be transmitted in small, relevant quantities, including all the necessary information from medical records and nothing extra. The FHIR standard can address this.
- Longitudinal analysis: This focuses on identifying patterns, trends, and predictors. Since these patterns are often complex, data from multiple systems and organisations need to be aggregated, collected, or compared to make reliable conclusions. The OMOP standard can cover this.
Detailed overview of healthcare data standards
OpenEHR is an open standard specification in health informatics that uses a two-level modelling approach—informational and knowledge-based—to facilitate flexible and consistent data management. By using predefined structures, OpenEHR ensures accurate data capture and sharing.
A centralised database with a tree structure allows for retrieving a complete patient record. The database schema is built on reusable archetypes and templates: patient-centric and clinical, and DB schema is extensible by design.
FHIR (Fast Healthcare Interoperability Resources) is a standard for exchanging healthcare information electronically. FHIR data is organised into discrete resources, such as patients, observations, medications, and encounters, each with a defined structure and elements. This modular approach allows flexible and efficient data sharing across different healthcare systems. FHIR's use of modern web technologies, like RESTful APIs, makes it easy to implement and integrate.
OMOP (Observational Medical Outcomes Partnership) is a standardised data model designed to facilitate healthcare data study from diverse sources. Data in OMOP are organised into a common data model (CDM) with tables representing different healthcare domains, such as patients, drugs, conditions, and procedures, allowing for uniform data representation. This standardisation enables efficient and consistent data analysis across various datasets.
OMOP's strengths lie in its ability to support large-scale observational studies, comparative effectiveness research, and real-world evidence generation. It is beneficial for researchers, hospitals and organisations looking to conduct systematic and reproducible healthcare data analyses.
ELEKS unified healthcare data management system solution
The EHDS regulations present the challenge of developing a health data platform that is interoperable, reusable, and compliant with standards. The suggested health data platform by ELEKS incorporates all required data classification types, processes, and modules to facilitate comprehensive operations in a medical institution and support the sharing and in-depth analysis of medical data.

Context diagram of the health data platform
The picture above illustrates the architecture diagram of a health data platform. This can be used for data storage, analysis, and transfer between health data systems. The platform combines three health data standards: OpenEHR, OMOP, and FHIR.
Diagram description:
- Data Sources: "Data Source 1", "Data Source 2", ..., "Data Source N". These are the input data sources. The objective of the Raw Data Storage is to collect everything in raw form.
- Raw Data Storage: Collect raw data from multiple data sources. Acts as a central repository for initial data collection before processing.
- OMOP Storage: An analytics storage system. It consists of a vocabulary mapping module and a data table mapping module and uses a "Common Data Model" to standardise data. It is the basis for various systems that analyse data, such as Data Science, Artificial Intelligence, and Data Analytics.
- OpenEHR Storage: The goal is to collect data and store it in a standardised format. Contains the "Information Data Module" and "Knowledge Data Module". Flexible and consistent data management through predefined structures. Transfers data to Primary and Secondary Use Systems using FHIR.
Azure healthcare data platform implementation
The context diagram of the data health platform above describes the general architecture of a health data platform that is not connected to any technology. For instance, by leveraging Azure services, the platform can be effectively implemented as follows:
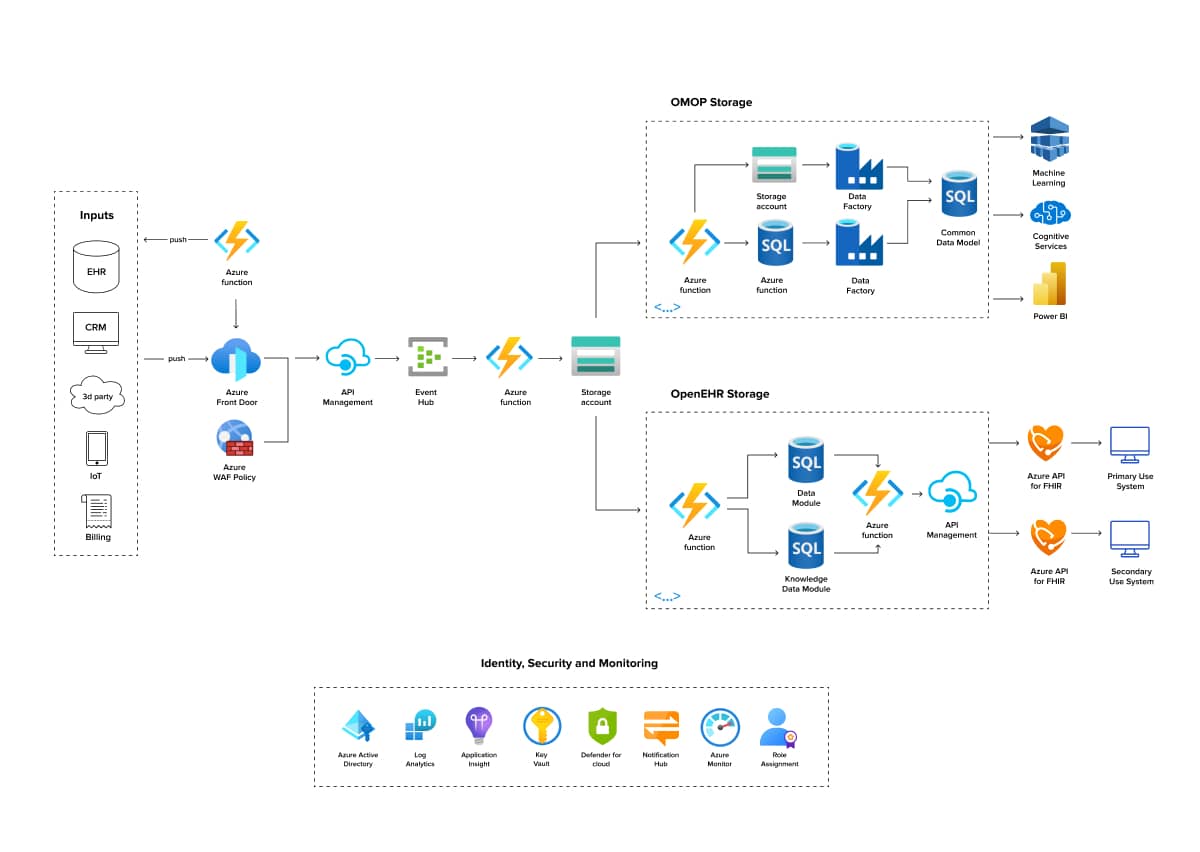
Azure health data platform
Data from multiple input sources is either pulled via Azure Functions or pushed through Azure Front Door, which integrates with Azure WAF Policy for security. The data is managed through API Management and directed to an Event Hub, from where Azure Functions writes the data into a Storage Account. The Storage Account acts as a centralised repository for further processing into either OMOP or OpenEHR storage.
In OMOP storage, data is transformed and standardised using the Data Tables Mapping Module and Azure Data Factory. Processed data is analysed through Machine Learning, Cognitive Services, and Power BI. In OpenEHR storage, data is managed through Information and Knowledge Data Modules, facilitated by Azure Functions and API Management, and transferred to primary and secondary use systems via Azure API for FHIR.
The platform also integrates Azure's Identity, Security, and Monitoring services, including Azure Active Directory, Log Analytics, Application Insights, Key Vault, Defender for Cloud, Notification Hub, Azure Monitor, and Role Assignment, ensuring secure and efficient operations.
Conclusions
The EHDS framework unifies health data exchange across Europe. By using standards like OpenEHR, FHIR, and OMOP, the proposed health data platform can overcome interoperability challenges, improve data quality, and ensure data security. The use of Azure services shows that modern cloud technologies can help build a flexible, secure, and efficient health data system. The suggested unified health data management platform can support EHDS' goals and improve access to advanced data analytics and better patient outcomes throughout Europe.

FAQs
Data in healthcare refers to any information related to patient health, medical history, treatment plans, outcomes, and operational metrics within healthcare organizations. This includes clinical data, administrative data, and financial data.
Data models in healthcare are structured frameworks that define how data is organised, stored, and managed within healthcare systems. They enable the integration and analysis of various data types from multiple sources, supporting decision-making and improving patient care.
The three V's of healthcare data are Volume (amount of data generated and collected), Velocity (the speed at which data is generated and needs to be processed), and Variety (the different types of data, including structured, unstructured, and semi-structured data).
Related Insights






The breadth of knowledge and understanding that ELEKS has within its walls allows us to leverage that expertise to make superior deliverables for our customers. When you work with ELEKS, you are working with the top 1% of the aptitude and engineering excellence of the whole country.

Right from the start, we really liked ELEKS’ commitment and engagement. They came to us with their best people to try to understand our context, our business idea, and developed the first prototype with us. They were very professional and very customer oriented. I think, without ELEKS it probably would not have been possible to have such a successful product in such a short period of time.

ELEKS has been involved in the development of a number of our consumer-facing websites and mobile applications that allow our customers to easily track their shipments, get the information they need as well as stay in touch with us. We’ve appreciated the level of ELEKS’ expertise, responsiveness and attention to details.

